If you're reading this there's a strong chance you, or someone you know has Achilles tendonitis. And as a Physiotherapist I completely understand how frustrating it can be.
This type of Achilles pain can be hard to shake quickly and can genuinely persist for months.
As an industry, we do a really good job of managing and treating Achilles tendonitis. Yet for all our hard work we're yet to collectively evolve to a point where we can consistently prevent it. Truth be told, I don't even think our collective understanding of its origin has progressed beyond injury-related cliches like overuse and bad luck.
In this article, I hope to help you better understand why your Achilles tendon has become sore and why it may not be progressing as it should.
So if you're struggling with Achilles tendonitis - or any other non-contact Achilles injury for that matter, let's discuss what you may be missing.
Achilles Tendonitis
The Achilles tendon is one of the biggest and most robust tendons in the body. Yet it's estimated over 1,000,000 people a year suffer an Achilles tendon injury.
While Achilles tendonitis* is clearly it's own condition, it's worth noting that its predisposing factors may be similar to other Achilles-related pain and injury. Just the consequences may differ.
*Note: At this point, it's important to reinforce that the word tendonitis is technically incorrect. '-itis' is used to indicate inflammation, however, the tendon dysfunction associated with tendonitis is not inflammatory. The correct term is tendinopathy which can be confusing if you hear different terms for the same condition. So for the purpose of this article, I'll keep it uniform and stick with tendonitis.
Achilles Tendonitis Cause
We typically look at the heel pain associated with Achilles tendonitis is an overuse injury.
It has an association with running, sprinting and jumping. The idea is that too much dynamic use can challenge your Achilles to the point of dysfunction. And it makes perfect sense on a number of levels.
However, from my perspective, I've always had an issue with "overuse" as an explanation for injury.
Interestingly, an old study from way back in 1997 suggests that approximately 31% of Achilles tendonitis occurs in people who aren't rigorously active. And as I've discussed previously with knee tendonitis the idea that too much use can cause injury is a little paradoxical.
By definition, use is entirely normal. It's what our tissue is designed for. Yet we seem happy to concede that your Achilles is now sore because you did the one thing you're supposed to do with it.
Let's not forget that most develop Achilles tendonitis on just the one side. Those who have bilateral tendonitis usually have one side worse than the other. So by filing this under overuse, are we conceding that you use one side more than the other? This may loosely relate to jumping-related activities, but how can this be true for something like running?
To me, this disconnect suggests we're missing something, somewhere. And I think I can fill in the gaps.
Achilles Rupture
Clearly the worst-case scenario for an Achilles injury is a complete rupture - as Golden State Warrior Kevin Durant can unfortunately attest.
As with many injuries, we seem happy to divorce two similar issues from each other. We see Achilles tendonitis differently to a rupture, which does make sense of course.
But we should be having the same conversation about both when talking about the underlying mechanisms that lead to each injury. From my experience, it seems that the same mechanical flaws must be present to set both up to fail when they do. It's just the consequences are different. But we'll get to this later.
Achilles Tendonitis Treatment
We have many avenues of treatment for Achilles tendonitis with Alfredson's eccentric strength program one of the most common.

As you can see, it involves eccentric (lengthening under tension) strengthening for the calf and Achilles tendon. The exercise requires you to lift your heels up off the edge of a step with your good leg, and then lower yourself down with your painful side. You want to respect pain but need to forge on regardless.
The full eccentric strength program can take up to 12 weeks to remodel and restrengthen the area. Sound appealing?
If it works, why not, right?
Other treatments typically include massage, taping, heel lifts in shoes, rest, anti-inflammatories and ice. We may even suggest you use an Achilles tendon brace.
If strength, conditioning, and these other techniques fail to solve your Achilles tendonitis you may then become a candidate for surgery.
But the problem I have with our current approach is that it often lacks context.
A sore Achilles tendon definitely needs treatment, but what about the rest of the leg?
After all, you aren't just an Achilles tendon floating independently through space. You're a living, breathing, sophisticated piece of organic machinery with a faulty part. It is connected to, and influenced by a large number of other joints, soft tissues, nerves, and vessels. Things that are designed to function happily within an established equilibrium.
So in order to treat a sore Achilles properly, we need to take a step back and find the broader issues in play.
What is setting your Achilles tendon up to fail?
The Mechanical Cause Of Achilles Tendonitis
From my clinical experience, Achilles tendonitis has almost everything to do with how we load the Achilles tendon, not just load in general.
To put things simply, the Achilles tendon likes to be loaded relatively vertically.
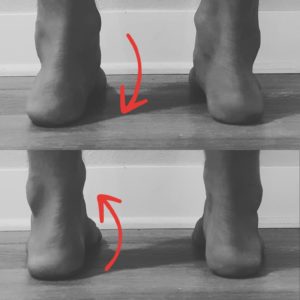
This can be seen really well when looking at someone from behind.

Good standing, walking and squatting mechanics will keep the Achilles relatively straight up and down.
Can you guess what causes the change in orientation above?
Two Overlooked Mechanical Faults With Achilles Tendonitis
From my work as a Physiotherapist, the following two factors seem to create poor loading associated with Achilles tendonitis.
1. Ankle Stiffness
This may not come as a surprise. However, it might if you don't realize your ankles are stiff.
Mechanically, ankle stiffness forces your entire leg to compensate as it tries to find a workaround. If you don't have the immediate range of motion your body needs to complete simple movements, it'll go looking for it somewhere else. We're talking feet that rotate out and knees, shins, thighs, and hips that rotate in. All as an attempt to find the path of least resistance around ankle stiffness.
Not only this, but ankle stiffness directly compromises the Achilles' ability to absorb shock. Less give in the ankle joint means less available give for the Achilles. Think rusty spring as opposed to a fresh new one.
The Role Of Modern Footwear
As human beings, it's hard to make sense of things we aren't paying attention to. We blame age for the innocuous aches and pains we accrue as the years go by - despite this being counterintuitive. If we wake with morning pain, we're inclined to blame a poor sleeping position, mattress and/or pillow rather than looking at the bigger picture. This is potentially part of the reason why most mechanical issues persist.
With this in mind, it's worthwhile noting that most ankle stiffness is the result of modern footwear. Our love of heeled shoes has a tendency to rob us of full ankle range of motion. So much so that any heel should be thought of as the exact amount of ankle range you don't get access to.
As the saying goes - you use it or lose it. And we're losing it without question.
I've gone into detail with this and what makes a good shoe before, but the addition of the heel is absolutely not one of them. I'd argue it's one of the single worst pieces of modern "technology" going around.
So the key here is to understand that modern heeled footwear can often set our ankles up to be stiff - with potentially nasty ramifications for the Achilles.
2. Tightness At The Front Of The Hip
It's a similar story if the front of your hip is tight.
Anterior hip tightness will again force the leg to move abnormally around a restriction. This is often characterized by walking with your feet turned out.
And you can easily feel this on yourself.
When walking, take a look at where your feet point. If they turn out, try straightening them up.
By doing so, you may expose any tightness at the front of your hip as your back leg trails behind. The bigger the step the more prominent it may be. If you let your feet turn out again that tightness should subside.
Your body will consistently make this decision on your behalf if the front of your hip is tight. Every single step.
The Role Of A Sitting-Based World
If you've been playing along over the years you'll appreciate how disastrous sitting can be for anterior hip mobility.
Nothing screams tight hips like spending hours a day with them bent in the same shape. Again, 'use it or lose it'.
The mechanical ramifications of this can filter all the way down to your Achilles tendon over time.
The Role Of Flat Feet
If you have a keen eye, you'll notice the collapsed arches in the previous image. Flat feet de-orientate the Achilles tendon leaving it vulnerable over time.
Interestingly, I've deliberately avoided referencing flat feet directly until now. And for one reason.
Collapsed arches are often the consequence of the same inward leg rotation associated with Achilles tendonitis. They go hand in hand.
Not because flat feet cause Achilles tendonitis, but because the same broad mechanical faults seem to create both.
This is another potential example of us failing to see the bigger picture.
If you take your shoes off you can observe this for yourself.
Without letting your feet lift, gently rotate your knees inwards and outwards. As you do this, you should notice that your arches will lift when you rotate your knees out and will collapse when you let your knees rotate in.
The image above highlights this. The flat arches in the top half of the image are magically replaced by stable and strong arches just by creating an outward rotational force through the leg.
With this in mind, you can hopefully appreciate how Achilles tendonitis (and even a ruptured Achilles) is more than just an Achilles tendon injury.
New Achilles Tendonitis Stretches To Consider
When it comes to treating the Achilles, consider adding these to your current Achilles tendonitis home treatment.
Remember, as we've discussed previously consider moving away from basic passive stretch holds, and instead use Power Bands and the more active PNF stretching technique.
- Banded Ankle Stretch:
The best way I've ever seen to improve ankle flexibility quickly is with a power band. Obviously stretching with a strong band can tug on a sore Achilles so pay attention to how it feels. Having said that you should be able to find a deep capsular stretch without pain.
- Couch Stretch:
The Couch Stretch is brilliant. In a lot of ways, it's the anti-sitting stretch as it targets those stiff hip flexors and quads. If you haven't done this before, go easy as it can be brutal. This can be made easier by doing it on a chair, or more challenging/beneficial with a powerband, but this time pulling forward.
- Pigeon Stretch:
With a leg that's consistently rotating inwards to go around restrictions, those hip external rotators (deep butt muscles) can become tight. By restoring better rotational mobility to your hips you can make it easier for your leg to stay "out" rather than collapsing in. If the ground doesn't work for you, use a table or bench instead, or another power band pulling laterally.
- Deep Squats:
You could possibly file this under strengthening, but there's a strong element of re-training here as well.
As you reclaim your missing mobility re-teach yourself to squat correctly. Re-train your hips to hold you in a strong, stable, externally rotated shape again.
Do this by keeping your feet straight and knees rotated out. This will pull those arches up and re-orientate the Achilles tendon.
Progressively load this shape with bands around your knees, weights, jumping and landing, and single leg work.
Strength is important but considering we've prioritized better mobility above, make sure you can put that mobility to better use.
- Foam Rolling :
Consider using a basic foam roller on your calf muscle. It's a great way to feed some slack into your Achilles tendon. It's also a nice alternative to stretching as you won't run the risk of annoying a sore tendon by pulling on it.
Similarly, spend some time mobilizing the front of your shin as well. This tissue is likely to be tight if it's been pulling against a stiff ankle for a while.
The restriction here contributes to ankle stiffness and further compromises the Achilles' ability to absorb shock. Again, feed some more slack to the back of the joint by freeing up the tissues that cross the front. Use a tennis ball or a grippy lacrosse ball for those hard-to-reach places.
Stand and Walk with Your Feet Straight:
To tie many of these concepts together, we also need to pay attention to the direction your feet point. Ankle stiffness and anterior hip restriction can cause a subtle shift in the orientation of your feet over time.
If you take your shoes off and look down, it's desperately important that your feet are straight. The more your feet turn out, the more your arches will collapse with every step.
Mobilizing your ankles and hips will certainly help, however, make the conscious effort to re-orientate your feet for the long-term health and function of your Achilles.
What Are the Best Shoes for Achilles Tendonitis?
The best shoes for Achilles tendonitis really depends on what your goals are.
If you're looking for a pair of shoes to help manage your symptoms, something with arch support and a slight heel is likely to do just that. Just be aware that you won't be addressing the underlying issues - just buffering them.
Arch-support will help stop the arch from collapsing, but it won't stop an arch from wanting to collapse. A raised heel will lessen the demands on the Achilles tendon but it will also create calf muscle tightness and ankle joint stiffness if left shortened for too long.
In a perfect world, we should always aim to feel comfortable in a good pair of barefoot or minimalist shoes. Interestingly, a minimalist shoe may absolutely exacerbate your Achilles tendonitis symptoms. However, this is not because minimalist shoes are bad for you. It's because their lack of support and heels are likely to expose the hidden underlying factors associated with the injury.
Realistically, the best shoe for Achilles tendonitis is the one that best supports your symptoms in the context of your life. If you just need to get by obviously go for something that helps your pain. Just know that if you aren't working towards feeling comfortable in a barefoot shoe eventually, then you may not be addressing the broader issues at play.
Final Thoughts
If you're dealing with any level of Achilles dysfunction and pain, take a step back and consider the bigger picture. Yes, the tendon is the source of your discomfort, but why?
My clinical experience tells me that ankle stiffness and anterior hip tightness must be explored if truly wanting to conquer the injury. By extension, you might want to reconsider the type of shoes you wear and your sitting habits.
If you don't, you run the risk of overlooking potentially key mechanical factors.
Please still prioritize your initial pain management, strength, conditioning, and general Achilles tendonitis treatment plan, but consider adding some broader mobility and re-training as well.
As with any injury make sure you have a trusted health professional work out what's specific to you.
If you can, you may not only speed up your progress but stumble onto a potential mechanical fix as well.
Good luck!
Frequently Asked Questions
Where is the Achilles Tendon?
The Achilles tendon is one of the strongest and most robust tendons in the body. It is part of a complex formed by the muscle of the calf and inserts into the heel bone.
What does Achilles Tendonitis feel like?
Achilles Tendonitis can often feel like a sharp pain with exercise and use.
Where does Achilles Tendonitis hurt?
Traditionally, Achilles Tendonitis occurs at the base of the tendon as it attaches to the heel or around the middle of the tendon.
Achilles Tendonitis is a consequence of poor overall leg mechanics. It is not just an Achilles tendon injury as per general perception. Tendons need to be used and loaded so rest is never the answer. In order to quickly settle your Achilles Tendonitis, it is important to free up any ankle stiffness, strengthen the tendon with eccentric exercises and improve your overall leg mechanics.
How long does Achilles Tendonitis take to heal?
Recovery from Achilles Tendonitis can vary based on its severity and the length of time before commencing treatment. General recovery can take 4-6 weeks once the tendon has been remodeled and loaded more appropriately. Chronic cases are common, mainly because the broader mechanical issues aren't addressed, or the tendon is not given an appropriate chance to settle.
Is walking good for Achilles Tendonitis?
The short answer is - it depends. Ultimately, Achilles Tendonitis is an issue with the way the Achilles is loaded over time, not that it is being loaded. With this in mind, walking is highly appropriate for Achilles Tendonitis as long as you have begun to improve the mobility of your ankle, the strength of your calf and broader leg mechanics. As always, your body will tell your Achilles is ready to tolerate degrees of walking.
This may sound obvious, but if walking genuinely increases your pain during activity, post activity, or the next day, then the exercise you did was beyond its current capacity to cope. At some point, walking will be fantastic but it's important to understand when that tipping point is.
Like many tendon issues, an untreated Achilles tendon injury may become a chronic injury. Unlike many general injuries, an Achilles Tendonitis is not cured through rest. It is not a condition where we need to wait for the tendon to settle. Instead, we need to go after the broader mechanical issues that caused the tendon to fail when it did.
How do I know if I've hurt my Achilles tendon?
Generally, the best way to tell if you've hurt your Achilles tendon is touch and feel it. If the tendon has become dysfunction you may feel a specifically tender or thickened spot. Similarly, you may need an Ultrasound or MRI to determine the extent or severity of any damage.
Absolutely. You should always expect your Achilles Tendonitis to go away. However, the catch is that you need to actively work on correcting the broader mechanical faults that lead the Achilles to become dysfunctional. This requires a proper assessment of your low back and entire leg to establish which areas are stiffer, tighter and weaker than they should be. Also, learning to squat and move correctly is a must. Ultimately, you should always have high expectations so long as you are working on the correct things.


1 comment
Hello! This is a great read – I am (was for the time being) an avid runner and have been dealing with chronic achilles pain in my right leg for the last 6 months, as well as some knee/hip soreness. I recently began to see a PT, who echoed many of the points you made throughout the article. I am curious as to what some good exercises for “mobilizing the front of the shin” are? This has been an area of emphasis for me but I’ve struggled to find stretches that do a good job of opening up the shin. Thanks!